Case report 1
DSM-TACE OF LIVER METASTASES FROM OVARIAN CANCER
REFRACTORY AFTER STANDARD THERAPY

Author: Roberto Iezzi, MD Fondazione Policlinico Universitario A. Gemelli, IRCCS
Università Cattolica del Sacro Cuore, Rome, Italy.
Patient
- 64 year old female
- Unresectable liver metastases from epithelial ovarian cancer
- Progress after two lines of standard chemotherapy (epirubicin, cisplatin, capecitabine)
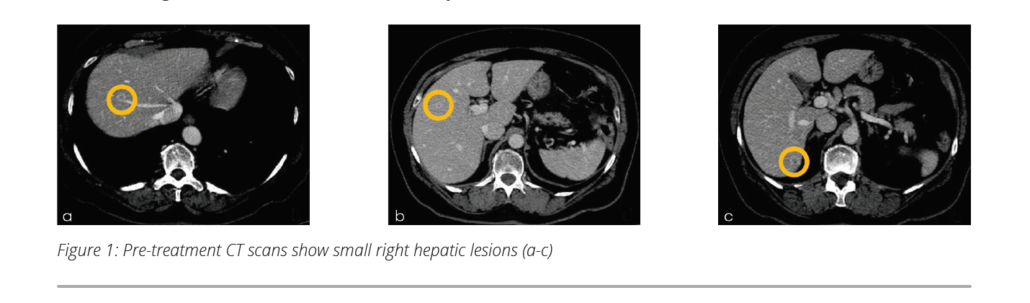
- Liver-only disease: multinodular, bilobar right hepatic disease (>5 lesions, <3 cm) | Fig 1a-c
- Lab parameters: Hb 12.7 g/dl | PLT 343×109/l | Leukocyte 6.5×109/l | Creatinine 0.9 mg/dl |
Prothrombin time 13 sec | INR 1.1| APTT 34 sec | ALT 45 IU/l | Serum bilirubin 0.8 mg/dl |
Serum albumin 38 g/l, normal range - Tumor board decision:
- DSM-TACE with Oxaliplatin and oral Cyclophosphamide (50 mg daily)
3 days after first intraarterial procedure - Bilobar treatment (two treatments at 2-week interval; the first treatment
was targeted to the lobe more involved by disease)


DSM-TACE Procedure
- Intraprocedural continuous infusion of 20 mg Morphine/24h, 20 mg
Ketorolac (NSAR)/24h, 500 mg Ciprofloxacin/once daily - DSM-TACE procedure was performed in an angiographic suite, using patient
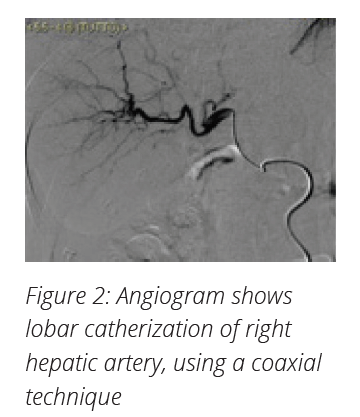
monitoring and anesthesiological assistance under local anesthesia - Anatomy of hepatic artery and possible branches to non-target structure
confirmed by hepatic angiography - Selective lobar catheterization was performed using 2.7 Fr
microcatheter | Fig 2 - Under fluoroscopic guidance, a solution of 450 mg in 7.5 ml of
microspheres type EmboCept® S* mixed with 100 mg Oxaliplatin
and non-ionic contrast medium was slowly infused in two steps: - Drug uptake: 100 mg Oxaliplatin diluted in 20 ml of 5% glucose solution plus 3.5 ml EmboCept® S*
plus 15 ml non-ionic contrast medium was injected - 4 ml of EmboCept® S* plus 6 ml non-ionic contrast medium was injected to obtain stop-flow.
- Endpoint for both steps was the delivery of the full planned dose with the achievement of an arterial stop-flow
Outcome
- Patient experienced mild nausea and abdominal pain, controlled and solved within 6 hours after
procedure with standard medical therapy - Patient was regularly dismissed after 24 hours, without any pain or periprocedural complications
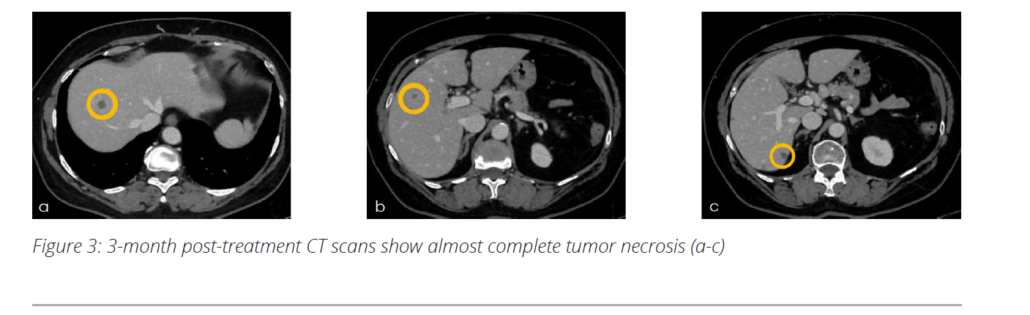
- 3-month CT follow-up showed an almost complete response with necrosis of almost all multinodular
hepatic lesions | Fig 3a-c
Outlook
- Based on 3-month follow-up result, patient will receive 2 more DSM-TACE sessions
CONCLUSION
- DSM-TACE causes a temporary occlusion with a short ischemic period, allowing for an optimal drug
uptake with no post-embolic effects, with a consequent optimal safety profile - The use of DSM-TACE offers an effective treatment option for patients refractory to standard
chemotherapy regimen, combining the locoregional treatment with a systemic chemotherapy, with
low drug-related toxicities.
